High Cholesterol Treatments: Does New Equal Improved?
Why It Matters
According to the Centers for Disease Control and Prevention (CDC), heart disease is the leading cause of death in the United States, killing more than 600,000 people each year – a total of one in four deaths1. By itself, coronary artery disease (CAD), the most common type of heart disease in the United States, costs the U.S. $108.9 billion each year2. As a result, tackling this condition has become a critical goal for U.S. healthcare providers.
Clinical Background
Also known as coronary heart disease, CAD is caused by plaque buildup in the walls of the arteries that supply blood to the heart and other parts of the body. Plaque is made up of deposits of cholesterol and other substances in the artery. Over time, this buildup causes the inside of the arteries to narrow, potentially blocking the blood flow. In the past, guidelines to prevent CAD suggested patients achieve a low density lipoprotein (LDL) level < 100 mg/dl, which limits the formation of plaque on coronary arteries. Newer guidelines do not address a targeted LDL level, but target the types of patients who should lower their LDL levels.
History of Treatments
For the past three decades the mainstay of treatment for CAD has been statin therapy. According to several national guidelines, statins are recommended as first-line therapy because they have the most convincing data for primary prevention, especially for higher risk patients. Statin therapy also has been recommended for secondary prevention in all patients with known cardiovascular disease or the risk equivalent.3
Newer so-called “high-intensity” statins were developed that had even more success in lowering LDL levels. Additionally, Zetia® (ezetimibe) was approved in the class of cholesterol absorption inhibitors which, when used alone or with a high-intensity statin, have proved effective in those patients with extremely high LDL levels.
A meta-analysis of more than 90,000 participants determined that reducing LDL levels by an average of 39 mg/dL will yield a 23 percent reduction in cardiovascular risk over five years.
Cost Effectiveness
In a study entitled “Cost-Effectiveness of Statin Therapy for Primary Prevention in a Low-Cost Statin Era,” Dr. Lawrence Lazar, et al. concluded that the use of low-cost generic statin therapy in the primary prevention of CAD was cost effective and suggested under certain conditions expanding to more aggressive prescribing would be cost effective in certain cases.4
This analysis used the benchmark of $4 per month for statin therapy, since the majority of statins are now generic. It’s important to note, however, that some of the high-intensity statins and ezetimibe are considerably more expensive, at approximately $250 per month. His study took into consideration the incidence of cardiovascular accidents, death rates and the costs of medical treatment associated with these events compared to the current low cost of statin therapies.
Adherence Challenges and Solutions
Statin medications are taken orally, usually once a day. Even with that simplistic schedule, many patients are non-adherent to these medications.
More than 30 years of research on statin therapies has shown that although most patients tolerate them well, a sub-population may be intolerant. However, recent studies indicate that patients who previously were intolerant to statins can tolerate them when reinitiated at a later time and possibly with a different agent. Researchers, such as Angela Pirillo and her colleagues, recommend managing statin-intolerant patients with alternative therapies, including switching them to another statin or the use of intermittent dosage regimens, as well as non-statin lipid lowering drugs (ezetimibe and fibrates).5
Oxford University researchers reviewed all articles regarding statin compliance. Their summary showed that poor adherence and discontinuation of statin therapy are a significant challenge. Their research indicates that, in the United States, it is estimated only about 50 percent of patients continue to take their statin therapy at six months, and 30-40 percent at one year.6 See Figure 1 for the data on percent of days covered (PDC), which is the most accurate way to determine a patient’s adherence.
Figure 1: Percent of days covered with statin
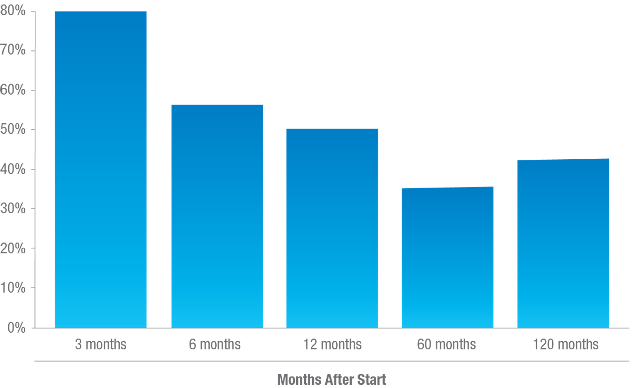
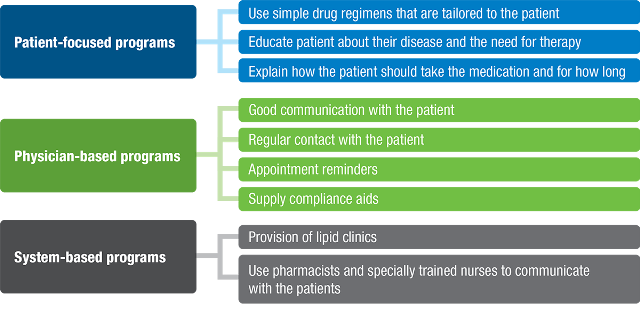
A study by DB Lawrence, et al. demonstrated that an adherence rate above 80 percent showed a significantly higher number of patients who were able to achieve a goal of < 100 mg/dl of LDL.7 The Oxford review also indicated that many adherence programs offered in the U.S. can have a positive effect on statin therapy compliance. See Table 1.
Table 1: Interventions to improve compliance with statin therapy
There is significant evidence that statin therapy is effective in lowering cholesterol and lowering the risk of CAD at a relatively low cost. The challenge is getting patients on statin therapy and keeping them on it.
New Therapies
This past summer, two new agents were approved by the FDA for certain cases of high cholesterol. These two agents, Praluent® (alirocumab) and Repatha™ (evolocumab), are in a new class of drugs called PCSK9 inhibitors. Praluent was approved as an adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia (FHC) or clinical atherosclerotic cardiovascular disease, who require additional lowering of LDL-cholesterol (LDL-C). Repatha was approved similarly but also includes an indication for homozygous FHC.
Evidence suggests these new agents can lower LDL levels significantly. The clinical studies showed a range of 32 percent to 60 percent reduction in LDL. While this is impressive, evidence from the use of high-intensity statin therapy with or without Zetia showed similar outcomes. The evidence available at this time does not correlate long-term cardiovascular outcomes data.
Potential Issues
Like any new medication, these therapies have drawbacks. These new agents are monoclonal antibodies which must be injected. Praluent must be injected every two weeks and Repatha can be injected either every two weeks or once per month. Adherence challenges could occur, given that these agents must be injected on an intermittent schedule. In addition, these medications carry substantially higher costs: approximately $1,400 per month vs. $4 per month for generic statins and $250 per month for certain high-intensity statins.
These new agents seem to be reasonably safe; however, they are not without adverse events. Issues such as neuro-cognitive disorders (i.e., amnesia and memory impairment), myalgia (muscle pain), disorders of the eye and some injection site reactions are possible. Additionally, these new agents are monoclonal antibodies, bringing up potential issues of more substantial adverse events that have not yet been identified.
Conclusion
Given the dramatic high cost and other potential drawbacks of these new PCSK9 inhibitors, the MedImpact approach will be to remain with statin therapy. Through appropriate patient support, statin adherence can be improved and – following the recommendations highlighted above – many patients can overcome intolerance issues. If there are adherence issues with the new PCSK9 inhibitors due to the fact they must be injected on intermittent schedules, payors will waste substantially more money than that spent on statin therapy. There may be some limited cases where these new agents could be utilized, but it would be prudent to wait to utilize these medications more broadly until after MedImpact has evaluated adherence in the real world, with long-term cardiovascular outcomes data, and gained a better understanding of the incidence of adverse events.
Steven G. Avey, RPh, MS, FAMCP
Vice President, Specialty Pharmacy Programs
Sources:
- Centers for Disease Control website August 28, 2015. http://www.cdc.gov/heartdisease/statistics_maps.htm
- Centers for Disease Control website August 28, 2015. http://www.cdc.gov/heartdisease/coronary_ad.htm
- Am Family Physician. 2011 Sep 1;84(5):551-558. Last, Allen R. MD, MPH. et al.
- Cost-Effectiveness of Statin Therapy for Primary Prevention in a Low-Cost Statin Era, Lazar, L D, et al., PubMed 2011 Jul 12;124(2):146-53. doi: 10.1161/CIRCULATIONAHA.110.986349. Epub 2011 Jun 27.
- Statin intolerance: diagnosis and remedies. Pirillo, Angela, et al. http://www.science.gov May 1, 2015.
- Oxford University http://www.medicine.ox.ac.uk/bandolier/aboutus.html
- Adherence to statin therapy and LDL cholesterol goal attainment by patients with diabetes and dyslipidemia. Lawrence DB, et al. Diabetes Care. 2005 Mar;28(3):595-9.
